
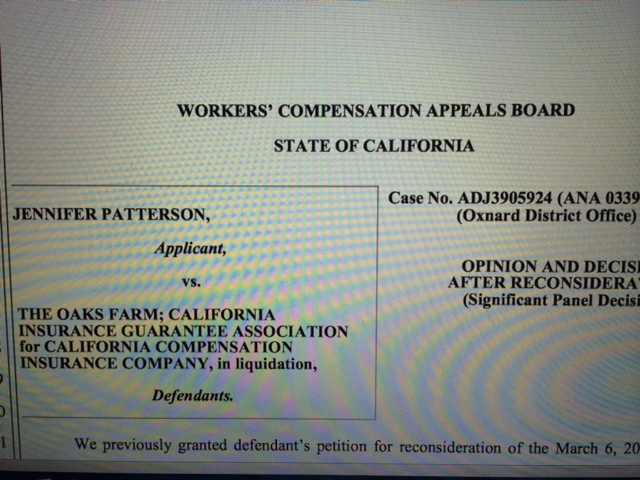
 California’s Workers’ Compensation Appeals Board has issued a new “Significant Panel Decision” today, Jennifer Patterson vs. The Oaks Farm and CIGA.
California’s Workers’ Compensation Appeals Board has issued a new “Significant Panel Decision” today, Jennifer Patterson vs. The Oaks Farm and CIGA.
Patterson is notable in various respects. First, it is the first major decision authored by new WCAB Commissioner Kathy Zalewski.
Second, the decision is one of the first of which I’m aware that addresses nurse case management under California law. The WCAB panel (Zalewski, Brass, and Sweeney) find that “the provision of a nurse case manager is a form of medical treatment under Labor Code Section 4600”. As a result, the entitlement to a nurse case manager can be addressed at an expedited hearing.
Third, the decision sets forth rules for when nurse case management services may be terminated. The panel holds that “An Employer May Not Unilaterally Cease To Provide Approved Nurse Case Manager Services When There Is No Evidence Of A Change In The Employee’s Circumstances Or Condition Showing That The Services Are No Longer Reasonably Required To Cure Or Relieve The Injured Worker From The Effects Of The Industrial Injury. “
Fourth, the decision clarifies whether a request for authorization needs to be used for continuing nurse case manager services. According to the panel, “It Is Not Necessary For An Injured Worker To Obtain A Request For Authorization To Challenge The Unilateral Termination Of The Services Of A Nurse Case Manager. “
Ms. Patterson apparently sustained a severe work injury to multiple body parts after being thrown from a horse in 1999. Nurse case manager services were authorized and provided by the insurer, but later unilaterally terminated. The report of the Agreed Medical Examiner had supported the need for nurse case manager services along with home health aide services.
It does not appear that defendant had ever been ordered to provide a nurse case manager, but rather had provided one voluntarily up to a point. The board noted that “when defendant initially provided nurse case manager services it effectively acknowledged that services were reasonably required to cure or relieve the effects of the industrial injury in this case.”
After a trial challenging the cessation of the nurse case manager, the workers’ comp trial judge had rendered a decision stating in part that “….there is no reasonable requirement for a Request for Authorization form for treatment that is in progress. Had the NCM services been stopped for a legitimate reason based on a medical opinion, and if a new need for the NCM developed, an RFA might be appropriate. Such is not the case here. The nurse case manager was necessary when provided and remained necessary throughout the course of treatment to the present times”.
The board panel agreed. The Patterson panel appears to have been disturbed by the subjective rationale offered by defendant for cutting off NCM services (i.e. that the injured worker was “difficult to deal with”).
Here is the formulation by the panel:
“Defendant acknowledged the reasonableness and necessity of nurse case manager service when it first authorized them, and applicant does not have the burden of proving their ongoing reasonableness and necessity. Rather, it is defendant’s burden to show that the continued provision of the services is no longer reasonably required because of a change in the applicant’s condition or circumstances. Defendant cannot shift its burden onto applicant by requiring a new Request for Authorization and starting the process over again”.
Although this decision will please injured workers and their advocates, it may disturb some defendants. The logic of the decision would appear to apply to many forms of medical treatment where workers are accustomed to getting certain treatments and medications originally provided voluntarily by defendants.
This is particularly so under the current system where many workers are finding that long-provided treatments are now being subjected to UR (utilization review) and, if denied, then, to IMR (Independent Medical Review).
Recent statistics from the DWC and WCIRB show that pharmacy disputes comprise a large percentage of UR & IMR disputes. Many of those disputes involve medicines that have long been voluntarily provided. Many workers and doctors are very disturbed when the meds are cut off.
Under the logic of Patterson, it may be more difficult for an insurer to require a doctor submit an RFA to continue those medications.
In Patterson the insurer did not send the issue of the need for nurse case manager services to UR. But if a RFA (request for authorization form) is not required, then it is not clear that the UR procedures can be invoked.
The Patterson panel noted that “Applicant has no obligation to continually show that the use of a nurse case manager is reasonable medical treatment”.
The panel continued, noting that:
“Instead, once defendant authorized nurse case manager services as reasonable medical treatment, it became obligated to continue to provide those services until they are no longer reasonably required under section 4600 to cure or relieve the effects of the industrial injury. like all treatment decisions, that determination must be based upon substantial medical evidence.”
This is a decision which will reverberate throughout the comp community. The logic would appear to apply to a much larger universe of treatments than the narrow issue of case managers for chronic and severe cases. Whether that proves to be the case is unknown.
The decision in Patterson can be found here:
http://www.dir.ca.gov/wcab/SignificantPanelDecisions2014/PattersonJennifer.pdf
Stay tuned.
Julius Young
www.boxerlaw.com